Periodontal Disease
Periodontal disease is a chronic inflammatory disease caused by an imbalance of the natural bacteria that between your gums and teeth. It causes the destruction of the surrounding bone and soft tissue.
Table of Contents
What is Periodontal Disease?
Periodontal disease (periodontitis) is caused by bacteria that live in between your gums and teeth. It is a chronic inflammatory disease that can never be “cured”, only treated and managed like other chronic conditions such as cardiovascular disease or diabetes.
Healthy gums are usually firm and well adapted to your teeth, leaving only a small gap (also called a pocket) between the gums and the teeth. Our oral microbiome is a complex ecosystem of bacteria that live in equilibrium, similar to our gut microbiome. When you brush and floss, you clean the pockets, creating an environment for the “good” bacteria to thrive and eliminating the “bad” bacteria.
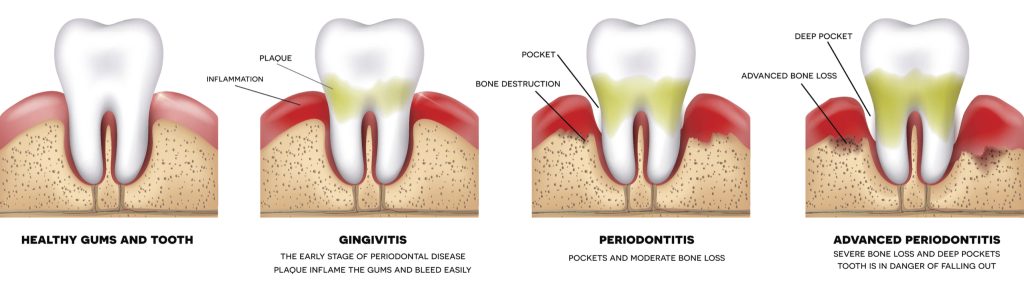
If plaque is allowed to accumulate around the gums long enough, it causes the gums to be inflamed. When the gums first become inflamed, it is called “gingivitis.” Inflamed gums are puffy and reddish, tender to touch or brush, and bleeds very easily. At this point, the damage is largely reversible with proper treatment and home care.
If the inflammation continues, it creates an environment that is beneficial to the “bad” bacteria to live and reproduce. This disturbance in the equilibrium or stability of the oral microbiome is called a dysbiosis. This dysbiosis is a negative feedback loop. The byproducts of the “bad” bacteria is poisonous to the gums and bone, creating more inflammation and causing the pockets to get deeper. As the pockets get deeper, they become more uncleansible and creates a more pro-inflammatory environment. As more “bad” bacteria continue to reproduce, more damage occurs to the gums and bone.
There are many factors that can influence the severity of periodontal disease. In particular, cigarette smoking and uncontrolled diabetes are strongly correlated with worsening periodontal health. Genetics can play a role – some people are more prone to periodontitis, and some forms of periodontal disease, such as aggressive periodontitis, can be inherited.
Periodontal disease and its destruction of the surrounding gums and bone cause many problems. Bone is the foundation that keep our teeth in our mouth. As bone is lost, teeth can become loose and unable to withstand the everyday forces of eating, chewing, and talking. In fact, periodontitis is the leading cause of tooth loss in the US. Bone loss around teeth make it more difficult to replace teeth with implants, as dental implants require the same bone support that teeth do. Dental implants can also be afflicted with periodontal disease, called peri-implantitis. Deep pockets are prone to getting acute infections and abscesses.
Periodontal disease also has a significant effect with our systemic health. As a chronic inflammatory disease, periodontal disease is strongly correlated with increased cardiovascular events such as stroke and heart attack. Periodontitis is linked to pre-term births and low birth weights in pregnant mothers. Bacteria found in our gums can cause infections in orthopedic prosthetics, such as knee and hip joint replacements, or artificial heart valves. Periodontal disease has been implicated in neurological conditions, such as Parkinson’s and Alzheimer’s disease – its pathogens have been found in the brains of patients with Alzheimer’s disease, which should be a sterile environment due to our blood brain barrier.
Periodontitis is largely an invisible disease. Most of the destruction that occurs to the gum and bone tissue is painless. By the time any symptoms occur, such as bad taste or foul smell from the gums, teeth loosening, or pain/discomfort, there has already been significant irreversible bone loss. The bacteria that cause periodontal disease live in a biofilm, so that antibiotics by themselves cannot get to them. Treatment requires mechanical disruption and removal of the biofilm.
What you should know before your Periodontal Disease Treatment in Orange County
Before scheduling for any treatment, you will first need a consultation. At this appointment, we will perform a comprehensive periodontal evaluation to assess the health and status of your gums and the underlying bone. During the evaluation, we will measure the depths of the pockets around the teeth, mobility of the teeth, and the inflammation of gums. If you have a general dentist that you see regularly and have recent x-rays then we will ask that you send a copy to us, or we can take them at our office. Dental radiographs are needed to evaluate what is happening underneath the gums – the teeth roots and underlying bone and other vital structures.
Once we have a full understanding of the current status and health of your periodontium, we can devise a plan together, and in combination with your regular dentist. We will discuss the prognosis of your teeth with and without treatment. We will discuss your treatment options and our recommendations, but our goal is to allow you to have a full understanding of your periodontal health and ultimately make the decision of how you wish to proceed with treatment.
We always strive to save your own natural teeth whenever possible and it makes sense to do so financially and in the overall treatment plan.
Non-Surgical Periodontal Disease Treatment
Scaling and Root Planing
Scaling and Root Planing (often called “deep cleanings”) is typically the initial treatment for periodontitis. When performed correctly with well-trained clinicians, like our dental hygienists and periodontists at Orange Periodontics, scaling and root planing can be a very effective treatment option. First, local anesthesia is used to numb the soft tissue and teeth to be treated. After profound anesthesia is achieved, the diseased root surfaces in the pocket are thoroughly cleaned and debrided of bacterial plaque and calculus (mineralized plaque and tartar build up) using hand instruments and ultrasonic instruments that vibrate at ultrasonic speeds to help break up biofilm. The root surfaces are smoothed out to minimize the plaque build-up and facilitate hygiene. Sometimes, scaling and root planing is combined with local or systemic antibiotics to help kill the “bad” bacteria and allows the oral microbiome to re-achieve homeostasis. The tissue is allowed to heal and re-attach to the roots for 4-6 weeks with meticulous hygiene and home care before we can re-check the area and re-measure the pocket depths.
A well-performed Scaling and Root Planing procedure accomplishes several things. In many cases, it can resolve the pocketing and gum inflammation so that no additional surgical treatment is needed, or at least get enough improvement that the disease can continue to be managed non-surgically. This is especially the case when the disease is more mild without significant bone loss. Even without complete resolution, scaling and root planing will reduce the number of sites that require surgical treatment, and allow the gums to be healthy enough for minimally invasive regenerative surgical treatment.
Periodontal Maintenance
Periodontal maintenance is a professional cleaning. It is similar to a dental prophylaxis, but a prophylaxis is only for those with healthy gums or gingivitis. Patients who have periodontal disease are always at risk for the pockets t. Periodontal disease cannot be cured, it is a chronic condition that is managed, like diabetes or heart disease. Often, we recommend periodontitis patients be placed on a shorter recall for professional maintenance visits, usually every 3-4 months. We may alternate these appointments with your regular dentist. At these visits, we re-measure the gum pockets to make sure they are stable. Especially if the pockets are a little deeper, we clean to the bottom of the pocket, deeper than you are able to at home. Periodontal maintenance is essential to the management of periodontal disease. By cleaning out the pockets every few months, we minimize the inflammation and keep the environment beneficial for our “good” bacteria to keep the pockets stable. If there are changes or worsening sites, we will detect it early enough before too much damage can occur and can manage it, either surgically or non-surgically. We will be able to see which areas need additional TLC and coach you on how you keep it clean at home. For most periodontal patients, the best thing you can do for your gums is brush and floss the best you can at home, and have professional periodontal maintenance visits every 3-4 months.
Surgical Periodontal Disease Treatment
Open Flap Debridement / Osseous Surgery
Gum flap surgery, also called open flap debridement, osseous surgery, or pocket reduction surgery, is a surgical treatment modality for periodontal disease. It is often performed when there are residual pockets after initial non-surgical treatment (scaling and root planing). This is because non-surgical treatment has limitations in how deep we are able to reach. When the pockets are too deep to access the bottom of the pocket, to fully debride the diseased root surface or reach the bony defect, surgery is needed to open the gums (open flap) to fully access and treat accordingly (debridement).
First, local anesthesia is used to numb the soft tissue and teeth to be treated. After profound anesthesia is achieved, the gums are carefully flapped away from the teeth and bone, exposing the bony architecture and root surfaces to be treated. With full access to the roots, the area can be thoroughly debrided and infected tissue cleaned away. Periodontal disease often leaves destructive crater defects in the bone. If left, these craters will not let the pocket to heal and will allow the “bad” bacteria to hide and grow. Because of this, the bone architecture is re-shaped and re-contoured (osseous surgery) to allow the gums to lay smoothly, excess diseased gum tissue is trimmed away to reduce the pocket, and the gums are sutured back in place. Often, biologic agents and proteins, such as Straumann Emdogain, made up of proteins called amelogenin, an enamel matrix derivative, is added to help the gums healthily reattach to the teeth to reduce the pocket.
Guided Tissue Regeneration and Bone Grafting
Periodontal disease causes destruction of the supporting bone and tissue around our teeth. With the newest developments in cutting edge biomaterials and microsurgical and minimally invasive techniques, we can now predictably regenerate lost bone and tissue better than ever.
Regeneration is centered on a few important biologic principals: a stable wound, and recruiting bone cells to repopulate lost bone, and soft tissue cells to repopulate lost tissue, and for the bone and tissue to attach back onto the previously diseased root surface.
In order to create the most stable wound and fibrin clot, we use minimally invasive surgical techniques with high magnification. When we perform regenerative surgeries, we use microsurgical blades and 5.5x magnification to create the smallest incisions while still being able to access and visualize the bone and root. Bone graft materials are mixed with biologics and growth factors and placed into the bony defect to regrow the bone. See our bone grafting page to learn more about bone grafts and where we source it from. Unfortunately, it takes much longer for bone to grow and mature, so we need to keep soft tissue from growing into the space. We do this by placing a bioabsorbable/resorbable barrier membrane over the bone to keep the soft tissue from growing into the bone (guided tissue regeneration). The finest microsurgical sutures are used to gently and precisely bring the tissue together for a stable wound.
Periodontal Disease treatment recovery and results: what to expect
After non-surgical treatment, especially scaling and root planing, your gums may be sore for a couple days. Any discomfort can usually be resolved with ibuprofen (Advil) or acetaminophen (Tylenol). You may experience some sensitivity to cold food and beverages, which should get better on its own with continued oral hygiene. After your treatment, it is imperative that you have meticulous home care. That includes brushing and flossing and using any tools we may have given you. We need the gum pockets to remain as plaque free and clean as possible to give them the best chance to heal and reattach. Your gums may bleed when you first start brushing, but it will lessen as you continue brushing. We will see you for a periodontal re-evaluation after 4-6 weeks and re-measure the gum pockets.
After surgical treatment, you will have dissolvable stitches in the area. Depending exactly what stitches are used, they may fall off in around a week or we will remove them at your post-operative appointment. You will be instructed not to brush or floss the surgical sites until we see you for the post-operative appointment as to not disturb the initial healing. We will give you a special toothbrush to use at your post-operative appointment. Afterwards, it is imperative that you keep the areas as clean as possible. Studies show that the best regenerative outcomes occur when the area is kept as plaque free as possible. We will usually wait 3 months to allow the bone and tissue to regenerate and attach onto the root before re-evaluating the sites.
After any periodontal disease treatment, you will be placed on a shorter periodontal maintenance schedule for long-term management. You will need to have professional cleanings 3-4 times a year with periodontal examinations to ensure the pockets remain stable. If there are changes throughout the years, you may need additional scaling or root planing or surgical treatment to get the gums back to health.
Our team of periodontists specialize in both non-surgical and surgical periodontal disease treatment, and serve the communities of Orange County, including Orange, Anaheim, Fullerton, Anaheim Hills, Tustin, Placentia, Yorba Linda, Santa Ana, Villa Park and Garden Grove. Book your consultation today!
